Can scientists look at changes in your baby’s gut bacteria to predict their risk of celiac disease? The link between the gut microbiome, genes and risk of celiac disease.
Gluten, a protein found in wheat, rye and barley is the cause of celiac disease. When a person with celiac disease eats gluten, it triggers an immune reaction in the small intestine. This causes severe damage to the intestine.
People with DNA changes in HLA genes (aka DQ2 and DQ8 haplotypes) are highly susceptible to celiac disease. Normally, HLA proteins alert the immune system against harmful foreign bodies, such as viruses and bacteria. The mutated HLA proteins on the other hand, recognize gluten as foreign, mounting an attack.
BUT, not everyone with HLA mutations will develop celiac disease. This suggests other genetic or environmental factors are necessary to trigger celiac disease. Scientists believe the microbes in our gut can be one factor that can give us important clues for effectively treating celiac disease.
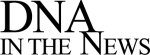
The critters in our gut
A very large community of bacteria and other microorganisms live in our intestines. The gut microbiome is established in the first two years of life, at around the same time our immune systemalso develops.
These microbes are an important part of our digestive health. They also play an essential part in shaping our immune reactions, by ensuring that our immune system will respond to harmful pathogens, but will remain tolerant to harmless components like proteins from our diet.
Balancing the gut microbiome
The composition of our gut microbiomes changes over time. Many factors such as changes in our diet, overall health and the use of antibiotics can affect this balance.
According to one recent study published in the journal of Gut Microbes, HLA mutations can also negatively impact the balance between good and bad microbes in our gut. Genetically predisposed babies have a higher prevalence of disease-causing bacteria very early on, which could potentially contribute to their risk of celiac disease.
Breast is best
The study looked at the presence of pathogenic bacteria and viruses in the stool samples of 127 babies at 7 days, 1 month and 4 months. All of them had a first-degree relative (a parent or a sibling) with celiac disease.
Formula-fed babies had a higher prevalence of Clostridium perfringens at all stages. C. perfringens bacteria are one of the most common causes of food poisoning in the US. At 4 months, a second gastrointestinal pathogen Clostridium difficile was also more frequent in formula-fed babies.
This is in agreement with already established findings that breast-feeding promotes healthy gut microbes, while formula feeding can alter the balance between protective versus pathogenic microbes. There is also evidence that disease risk is lower in babies who are still breast-fed when gluten is first introduced.
More bad bacteria in babies who are genetically predisposed
So, what role does genetic predisposition plays in the make up of the gut microbiome?
Babies at high genetic risk for celiac disease had more of the pathogenic bacterium Enterotoxigenic Escherichia coli in their stool. Enterobacteria are the leading cause of diarrhea in the developing world and the most common cause of traveller’s diarrhea.
Quite interestingly, the association held true for both breast and formula fed babies, implying HLA mutations may somehow affected the balance between healthy and bad bacteria in the gut.
Studies show, both breast-fed and formula fed babies with HLA mutations have lower numbers of the good bacteria. As such, the higher incidents of bad bacteria maybe a potential consequence.
Cause or consequence?
A fair bit of other evidence also supports a link between celiac and gut bacteria. Multiple studies show
- Celiac children have lower levels of good bacteria (e.g. Lactobacilli, Enterococci and Bifidobacteria) and higher levels of harmful bacteria (e.g. Salmonella, Bacteroides and Shighella) in both fecal and duodenal samples.
- A link between HLA-DQ2/DQ8 genotype and altered gut microbiome composition.
- Early bacterial and viral infections and the number of gastrointestinal infections contribute to celiac disease risk
The idea is that the microbial imbalance changes the environment in the intestinal tract, likely by elevating the levels of inflammatory proteins released by immune cells. This prolonged inflammatory reaction is what causes the harmful damage to the intestinal lining seen in celiac disease.
But, scientists are still not sure exactly how the gut microbiome and genetic predisposition affects each other. Future research is necessary to unravel this link.
Diet and probiotics to reduce the risk
Right now the only effective treatment for celiac disease is a strict gluten-free diet. When the environmental trigger is removed, the intestinal lining will usually recover, so normal absorption of nutrients can continue.
However, there are conflicting results on whether a gluten-free diet will restore the balance of the gut microbiome. Taking probiotics while following a gluten-free diet may potentially reduce both the intestinal inflammation and symptoms of celiac disease.
Future studies, like this one that track healthy babies with a family history of celiac disease, will hopefully one day give us the solution we need to identify new microbiome-based preventive and treatment options for celiac disease.